2025 AIChE Annual Meeting
(277a) Deciphering the Role of the Endothelial Glycocalyx in Alzheimer's-Related Neurovascular Pathology
Authors
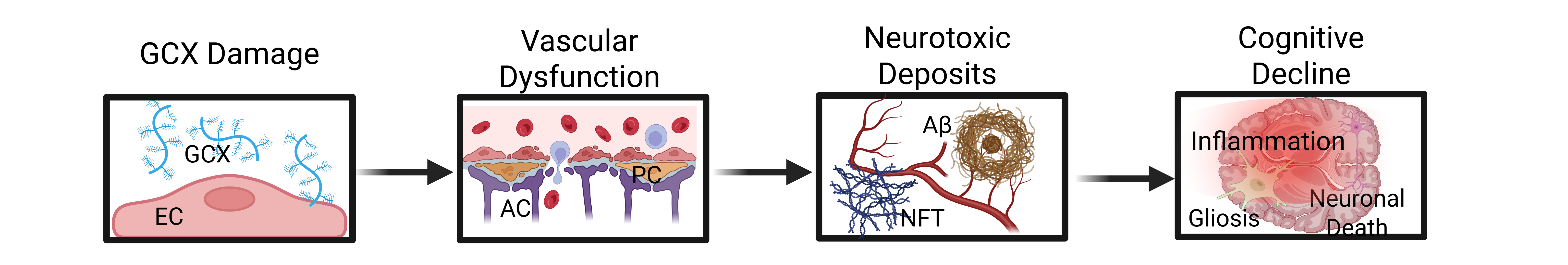
Alzheimer’s disease (AD), the most common form of dementia, currently affects over 55 million people worldwide, yet its precise etiology remains elusive (1). While amyloid-β and tau aggregates have traditionally dominated research efforts, recent studies suggest that blood-brain barrier (BBB) breakdown may precede and potentially drive downstream neuropathology (2,3). The endothelial glycocalyx (GCX)—a carbohydrate-rich structure on the luminal side of endothelial cells—is a critical but underexplored regulator of BBB integrity (4,5). Not only is the structure essential to vascular physiology, but postmortem analysis has shown extensive GCX degradation in AD brains compared to healthy controls, further motivating investigation (6). Notably, the individual roles of GCX components such as CD44 and Syndecan-1 (SDC-1) in BBB dysfunction remain unclear. We hypothesize that selective loss of these components impairs BBB function and contributes to early AD-related vascular pathology.
Methods:
A physiologically relevant in vitro BBB model using human cerebral endothelial cells (hCMEC/D3), astrocytes, and pericytes cultured on Transwell was developed (7). After forming a monolayer, endothelial cells were exposed to 12 dynes/cm² of laminar shear stress using a custom millifluidic device. CD44 and SDC-1 knockdown endothelial cells were induced via lentiviral transduction and confirmed by immunocytochemistry and western blotting. BBB function was evaluated through 3 kDa dextran permeability, tight/adherens junction protein analysis (ZO-1, VE-Cadherin), and AD-relevant transporters (GLUT-1, LRP1). ICC assessed junctional organization, GCX component shedding, and PECAM-1 continuity.
Results:
Stable, disease-relevant knockdowns of CD44 and SDC-1 (~50%) were confirmed and sustained across passages. Knockdown of either protein significantly increased 3 kDa dextran permeability (62% for CD44, 41% for SDC-1), indicating impaired barrier integrity. Western blots showed reduced ZO-1 expression (58% for CD44, 30% for SDC-1); only SDC-1 knockdown increased VE-Cadherin by 90%. CD44 knockdown uniquely decreased LRP1 (46%) and increased GLUT-1 (32%), with no such effects seen in SDC-1 knockdown.
Immunocytochemistry corroborated the expression trends observed in the western blot analyses. However, only CD44 knockdown disrupted ZO-1 membrane localization, increasing junctional fragmentation. Both knockdowns reduced their respective glycosaminoglycans—hyaluronic acid and heparan sulfate—and decreased PECAM-1 continuity, further supporting endothelial destabilization.
Discussion:
Our findings reveal that GCX components regulate BBB integrity through distinct, mechanistically important roles. While both CD44 and SDC-1 loss disrupted barrier function, CD44 knockdown had a more pronounced effect on junctional organization and transporter expression, suggesting it plays a central role in maintaining endothelial homeostasis under flow. The divergent responses in junctional and transporter profiles highlight how GCX degradation doesn’t act uniformly but instead alters specific pathways linked to AD-relevant dysfunction. These results support growing evidence that early vascular breakdown contributes to neurodegeneration (2,3,5,6).
This study strengthens the vascular hypothesis of AD and positions CD44 as a promising therapeutic target. By using a physiologically relevant, shear-adapted BBB model, we provide a platform for uncovering GCX-dependent mechanisms and accelerating translational research on barrier restoration in neurodegenerative disease.
References
- 2021 Alzheimer's disease facts and figures. Alzheimer's & Dementia. 2021;17(3):327-406.
- De la Torre JC, Mussivand T. Can disturbed brain microcirculation cause Alzheimer's disease? Neurol Res. 1993;15(3):146-53
- Sweeney MD, Sagare AP, Zlokovic BV. Blood-brain barrier breakdown in Alzheimer disease and other neurodegenerative disorders. Nat Rev Neurol. 2018;14(3):133-50.
- Tarbell JM, Cancel LM. The glycocalyx and its significance in human medicine. Journal of Internal Medicine. 2016;280(1):97-113.
- F, Zhong L, Luo Y. Endothelial glycocalyx as an important factor in composition of blood-brain barrier. CNS Neurosci Ther. 2021;27(1):26-35.
- Smyth LCD, Murray HC, Hill M, Van Leeuwen E, Highet B, Magon NJ, et al. Neutrophil-vascular interactions drive myeloperoxidase accumulation in the brain in Alzheimer’s disease. Acta Neuropathologica Communications. 2022;10(1).
- Harding IC, O'Hare NR, Vigliotti M, Caraballo A, Lee CI, Millican K, et al. Developing a transwell millifluidic device for studying blood–brain barrier endothelium. Lab on a Chip. 2022;22(23):4603-20.