Problem: Polyvinyl chloride (PVC) is the most widely used medical plastic, composing 75% of medical tubing globally produced in 2020 (BCC Research 2022), and its transparency enables visual inspection for clots. However, proteins readily bind to hydrophobic surfaces like those of PVC tubing. Furthermore, di-(2-ethylhexyl phthalate) (DEHP), a common plasticizer incorporated during the manufacture of flexible PVC tubing, may migrate to the tubing surface, causing it to become tacky and increase protein adsorption. Antifouling surface coatings for medical-grade PVC tubing provide a strategy to mitigate thrombosis and biofilm formation and reduce or eliminate the need for systemic anticoagulants. In this work, we aim to develop a superhydrophilic, non-heparinized, zwitterionic polymer coating to delay or prevent blood-plasma coagulation on PVC tubing used in extracorporeal membrane oxygenation (ECMO) circuits.
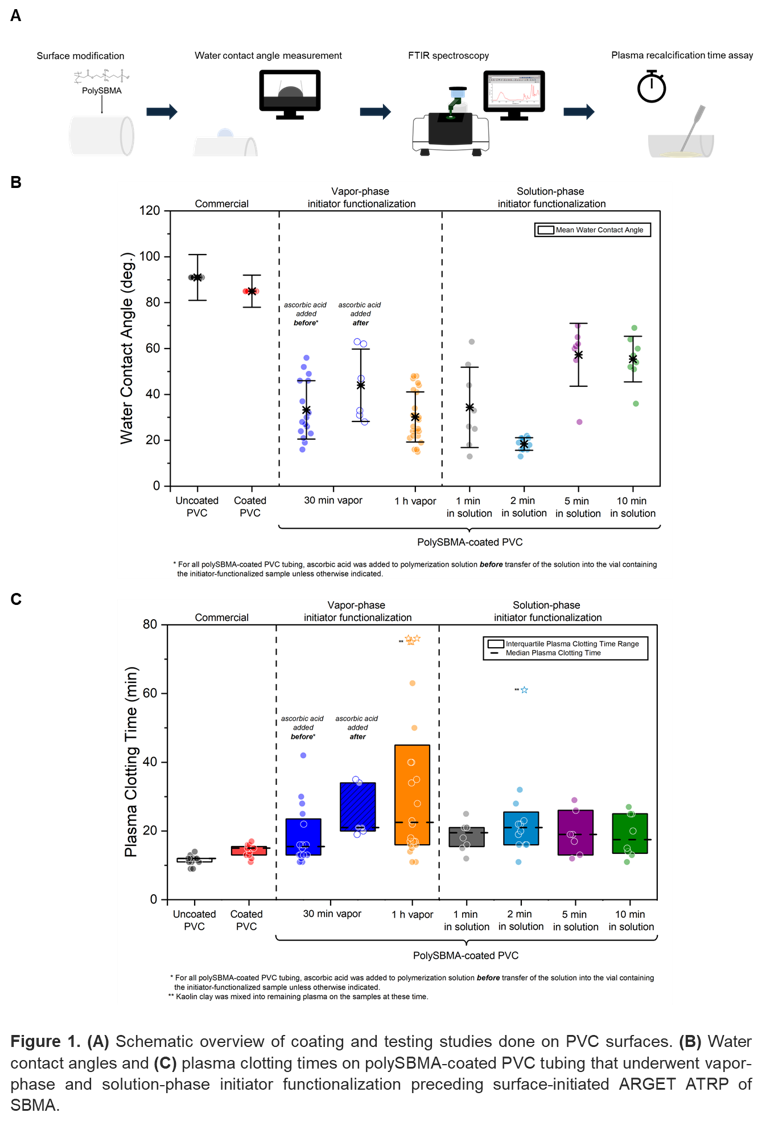
Methods: Atom transfer radical polymerization (ATRP), initiated by activators regenerated electron transfer (ARGET), was employed to produce zwitterionic poly(sulfobetaine methacrylate) (polySBMA) coatings on two brands of commercially available medical-grade PVC tubing. Solution-phase and vapor-phase approaches to initiator immobilization were explored to establish favorable conditions for producing polySBMA coatings with consistent properties. Chemical modification was validated by changes in wettability determined through water contact angle measurements. Changes in chemical composition and differences in coating thickness were investigated using attenuated total reflectance Fourier transform infrared spectroscopy (ATR-FTIR). Plasma recalcification time was assayed to assess the hemocompatibility of the polySBMA-coated PVC tubing under static in vitro conditions. For samples that did not clot after an extended time, procoagulant kaolin clay was added to determine whether sufficient clotting factors remained in the plasma for activation of the coagulation cascade. Clotting times on glass microscope slides served as a reference baseline for understanding how human plasma interacts with a polySBMA-coated surface.
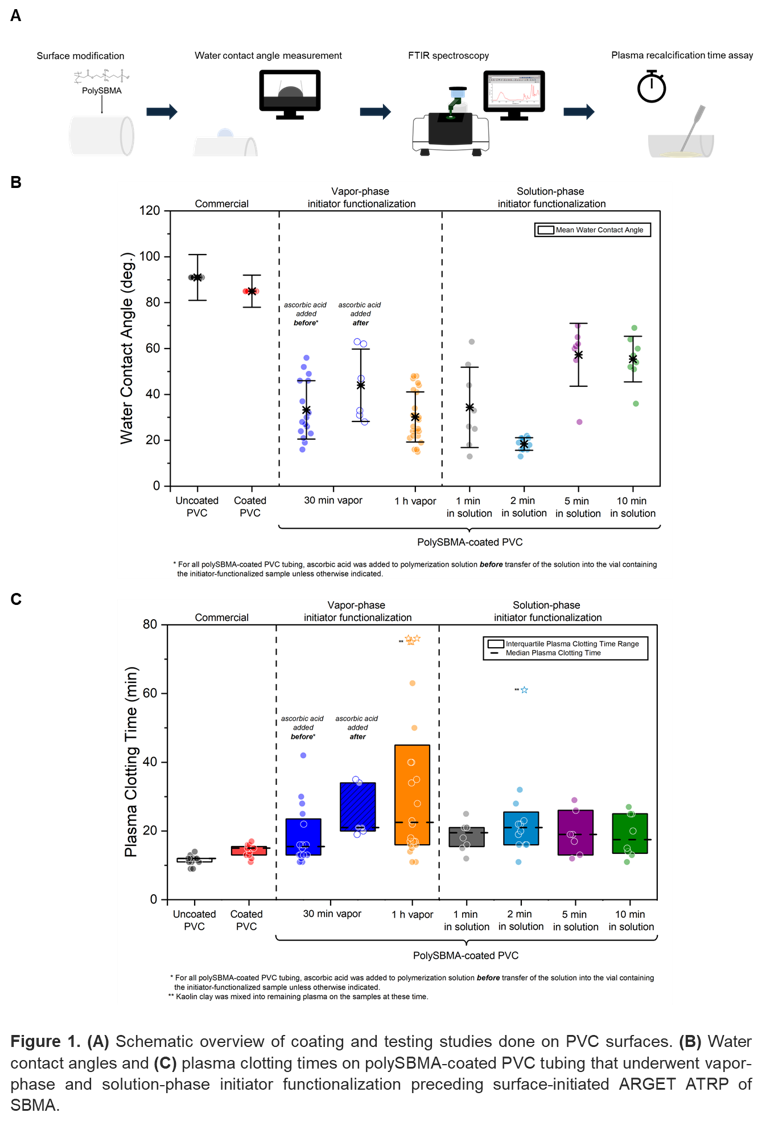
Results: PolySBMA-coating of a commercially available medical-grade PVC tubing selected for surface modification generally exhibited prolonged plasma clotting times compared to alternative commercially available options. Well-formed polySBMA coatings with consistently high wettability were achieved through a 2-minute solution-phase treatment to the initiator prior to surface-initiated ARGET polymerization of SBMA, while the longest plasma clotting times were observed on those resulting from 1-hour initiator vapor exposure prior to ARGET polymerization. The same procedures were applied to incorporate polySBMA coatings on PVC tubing from another vendor, and although surface wettability was increased, the tubing's already excellent clotting resistance did not improve, indicating a dependence on the PVC source and its manufacture.
Implications: This work demonstrates the practical functionality of polySBMA coatings in enhancing the antithrombogenicity of ECMO circuits. Owing to the curvature and optical transparency of the PVC tubing, which limited the use of traditional ellipsometry for measuring film thicknesses, variations in coating thickness were estimated from FTIR bands associated with sulfonate groups in polySBMA. Although wettability affects plasma protein-surface interactions, the uniformity of the thick polySBMA films on the PVC surfaces appeared to have a greater effect on plasma clotting time. PolySBMA coatings on PVC tubing examined in this work exhibited hydrophilicity and delayed coagulation times, albeit with some variability, demonstrating their potential efficacy as surface coatings. Further process development is necessary to replicate the properties of the polySBMA coatings on PVC across different manufacturers due to potential differences in tubing formulation.
Acknowledgement: We thank Dr. Justin Godown (formerly of Vanderbilt University Medical Center) for providing the commercial medical tubings; Dr. David Gailani (Vanderbilt University Medical Center) for providing the materials and supplies for the coagulation studies; and Dr. Maxim Litvak for his guidance on conducting the plasma recalcification time assays.